
Eleven nutrition experts react to the 2025–2030 US dietary guidelines





Coral Red: Mostly False
Orange: Misleading
Yellow: Mostly True
Green: True
Learn more about our fact-checking policies
The Dietary Guidelines (DGA) for Americans, 2025–2030 are being sold as a major reset of US nutrition policy, with a simple headline message: eat real food. The document is short, but it matters because US dietary guidance influences public programmes and the wider food environment, especially when translated into school meal standards and procurement choices.
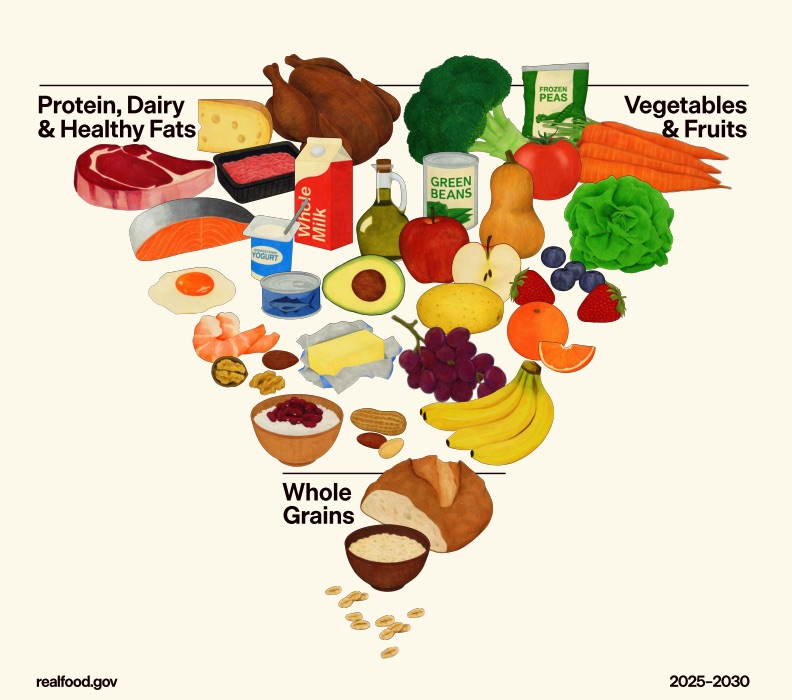
What’s grabbing attention worldwide is the new inverted food pyramid, which visually puts protein foods, dairy and fats at the top, while whole grains appear as a narrow base. Even before you get into the science, the visual itself signals a cultural shift: the “centre of the plate” looks more animal‑heavy than many public‑health models elsewhere.
This feature summarises what the new guidelines say, then shares reactions from credentialled dietitians and other nutrition experts (with translation where needed). It also flags where evidence is solid, where it’s contested, and where messaging may be vulnerable to political or industry influence.
What the 2025–2030 US dietary guidelines actually say
The guidelines repeatedly push Americans toward whole or minimally processed foods, protein foods, dairy, vegetables, fruits, healthy fats and whole grains, while urging a “dramatic reduction” in highly processed foods and sugary drinks. The document also includes life‑stage guidance (infancy through older adulthood) and notes that people with chronic disease may need tailored approaches under professional supervision.
Here are the most consequential points that have triggered debate:
- Protein target: 1.2–1.6 grams of protein per kilogram of body weight per day, with advice to prioritise protein at every meal.
- Dairy: three servings per day in a 2,000‑calorie pattern, specifically full‑fat dairy with no added sugars.
- Fats: a preference for oils like olive oil, but butter and beef tallow are also listed as options.
- Saturated fat cap stays: saturated fat should not exceed 10% of total daily calories.
- Ultra‑processed foods and sugar: avoid “highly processed” packaged foods (salty/sweet snacks) and avoid sugar‑sweetened beverages; the text states that no amount of added sugars or non‑nutritive sweeteners is recommended, and adds a practical cap of no more than 10 g added sugar per meal.
- Sodium: <2,300 mg/day for ages 14+ (with lower limits for children).
- Vegetarian and vegan diets: the document highlights potential nutrient shortfalls and advises monitoring key nutrients (e.g., B12, vitamin D, calcium, iodine) and using targeted supplementation if needed.
Leading International Nutrition experts react
James Brash, RD (London, UK)
James Brash is a UK-based registered dietitian working in the NHS (Scotland/UK), with a clinical background and an interest in clear public health messaging.
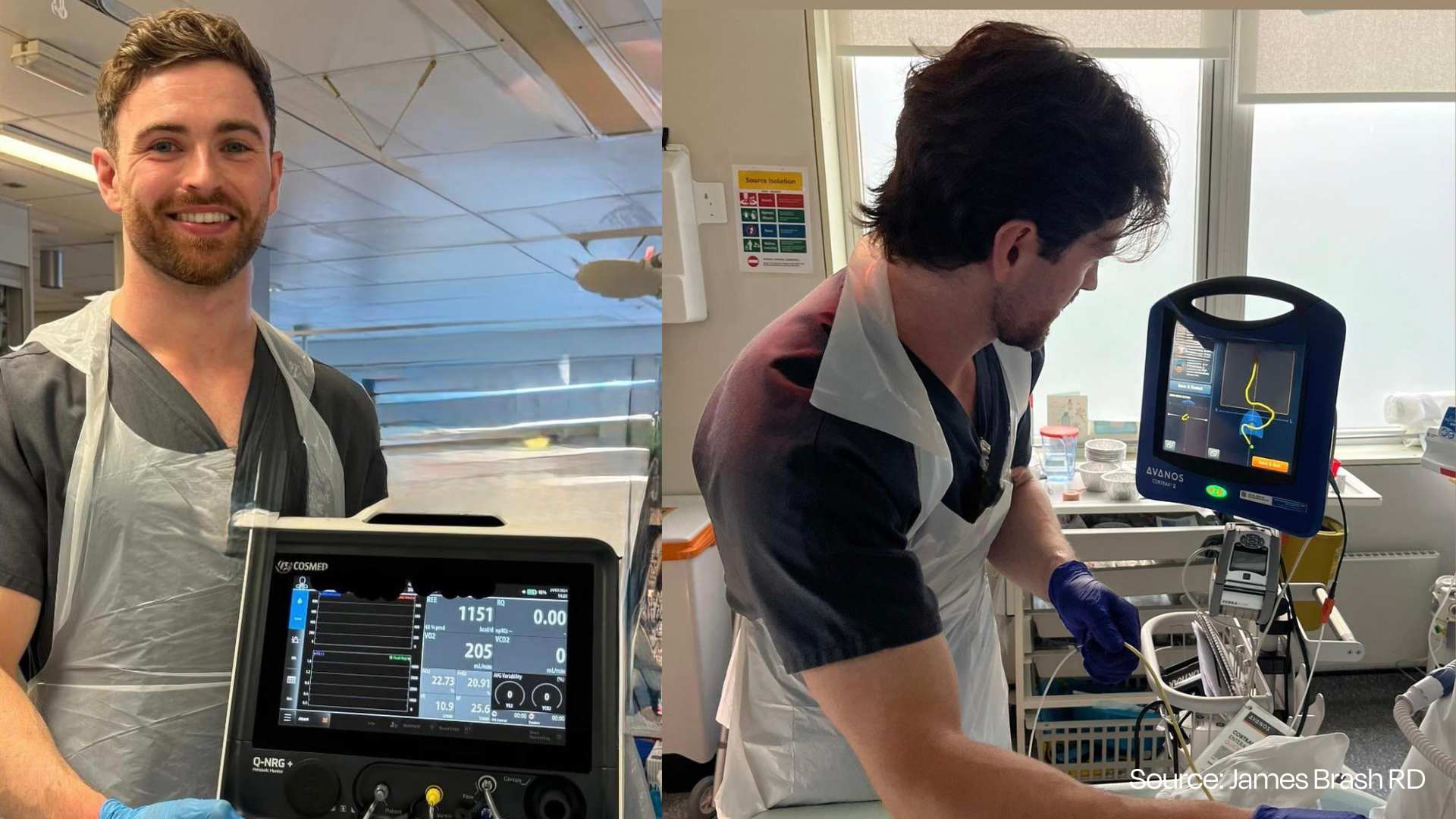
“The image is doing politics, not nutrition”
Brash’s main criticism is that the new US guidelines are being marketed as a dramatic overhaul, when much of what’s “new” is actually political framing and a headline-grabbing graphic. In his view, the public-facing images serve a narrative more than they serve public health, and the inverted pyramid doesn’t accurately reflect the written guidance.
He gives credit where it’s due: the broad message to eat more whole foods and fewer ultra‑processed foods is sensible and widely agreed.But he argues that this is being presented as a bold new direction even though it’s been standard advice for decades.
Why Brash thinks the pyramid creates confusion
Brash says the biggest problem is coherence. The text retains the long‑standing advice to keep saturated fat under 10% of calories, but the image places foods typically higher in saturated fat, like red meat, dairy and butter, high up on the pyramid, which sends the opposite signal.
He also points out that US nutrition problems are not driven by protein deficiency: most Americans already get enough protein, while far more people fall short on fibre. So he sees it as backwards that whole grains sit at the bottom of the graphic and beans/legumes are barely visible, even though they’re one of the easiest ways to raise fibre and improve diet quality.
Brash’s conclusion is that the new pyramid functions less like a practical nutrition tool and more like an ideological symbol, and that the likely outcome of mismatched visuals and messaging is public confusion, the opposite of what dietary guidelines are meant to achieve.
Roxanna Tosca, MS, RD, LND (Puerto Rico)
Roxanna Tosca is a Puerto Rico‑based dietitian (RD, LND). Roxanna Tosca on the Colegio de Nutricionistas y Dietistas de Puerto Rico team page.
In Spanish‑language coverage discussing the newly released 2025–2030 US guidance, Tosca strikes a more measured tone than many viral reactions. She warns that guidelines written for the US still need cultural adaptation before being applied elsewhere, saying different countries need to “llevarlo a su marco y su adaptación cultural” (bring it into their own framework and cultural adaptation).
She also pushes back against “good food/bad food” thinking. In the same piece, she stresses portion and frequency: it’s not the same for a child to eat one small piece of chocolate as it is to eat three bars. That framing matters because the new US pyramid is highly visual and easy to moralise—especially on social media.
“This guide… different countries need to bring it into their own framework and cultural adaptation.” (translated from Spanish)
Vandana Sheth, RDN, CDCES, FAND (United States)
Vandana Sheth is a registered dietitian nutritionist (RDN) and diabetes care and education specialist (CDCES), known for culturally inclusive nutrition guidance, including plant‑forward and vegetarian patterns.
In a LinkedIn post explicitly responding to the 2025–2030 Dietary Guidelines, Sheth resists the temptation to start with outrage. Instead, she highlights what she thinks the guidelines get right: continued emphasis on fruits, vegetables, fibre, and whole grains, plus the push to limit added sugars and ultra‑processed foods.
Sheth also frames the guidelines as a population‑level “direction,” arguing the real work happens when dietitians translate broad advice into strategies shaped by culture, preferences, health conditions, genetics and “real‑life context.” That’s a useful counterweight to the new inverted pyramid, which can feel like a one‑size‑fits‑all statement.
“Nutrition guidance works best when it creates a framework for progress, not rigid rules.”

Manuel Rodriguez, MS, RDN, LD (United States)
Manuel Rodriguez is a registered dietitian (MS, RD/RDN, LD). His professional profile describes clinical experience supporting people with chronic conditions such as diabetes, high blood pressure and kidney disease.
In a LinkedIn post explicitly titled around DGA 2025–2030, Rodriguez takes a practical, client‑centred stance: the guidelines aren’t “bad,” but they can be misread, especially if the pyramid graphic is treated like a literal ranking of what to eat most.
He also foregrounds affordability and realism. Rather than telling people to buy only fresh produce, he points to frozen or canned fruits and vegetables (with minimal added sugar/salt) as workable options for people on tight budgets—an important equity lens as these guidelines filter into institutional and household choices.
Katie Dodd, MS, RDN, CSG, LD, FAND (United States)
Katie Dodd (The Geriatric Dietitian) argues the new guidelines are less of a revolution for older adults and more a repackaging of long‑standing priorities: nutrient density, reducing ultra‑processed foods, and getting adequate protein across the day. She notes the new recommended protein range (1.2–1.6 g/kg/day) is a significant shift from older US messaging, and says many older adults may benefit from higher protein—while stressing that individual medical conditions still matter.
Dodd also flags the risk that the inverted pyramid could confuse people about whole grains and other categories, encouraging readers to pay attention to the written guidance rather than the graphic alone.
Jessica Corwin, MPH, RDN, NBCHWC (United States)
Jessica Corwin (quoted as an RDN in Good Housekeeping) questions whether returning to a pyramid—“even an inverted one”—will help people build meals better than simpler plate-based visuals. She also highlights a practical contradiction: the pyramid visually elevates foods often higher in saturated fat while the text keeps a saturated fat cap, which may be hard for the public to reconcile.
Her critique is fundamentally about implementation: confusing visuals can undermine public health guidance even when parts of the text are sensible.
Lindsey Schoenfeld, MS, RDN (United States)
Lindsey Schoenfeld (RDN and chef) applauds the guidelines’ clearer stance against ultra‑processed foods, refined carbohydrates and added sugars, saying she’s “thrilled that the focus is on real, whole foods.” Her response reflects a strong consensus point: reducing sugary drinks and ultra‑processed snack patterns is one of the most defensible, high‑impact public health messages in nutrition.
Schoenfeld’s angle is practical: cook more from basic ingredients and let “real food” mean something operational, less packaged snacking, more meals built from recognisable staples.
Lauren Harris‑Pincus, MS, RDN (United States)
Lauren Harris‑Pincus (RDN) supports reducing sugar but argues the guidelines’ “no amount” framing for both added sugars and non‑nutritive sweeteners is unrealistic and could leave people—especially those with diabetes or prediabetes—without practical options when transitioning away from high‑sugar patterns. Her core point is behaviour change: absolutist messaging can push people into all‑or‑nothing thinking, when measurable reductions (like cutting sugary drinks) are often more achievable and impactful.
This critique doesn’t deny harms of high added sugar; it questions whether the way the guidelines talk about sweeteners will help people change, or simply make them feel they’ve failed.
Stephanie Hodges, MS, MPH, RDN (United States)
Stephanie Hodges (RDN; public health and policy) cautions that the guidelines include recommendations that align with nutrition research and others that do not, and reminds readers that “guidelines are just that: guidelines.” Her emphasis is on what happens next: the document’s real-world influence will show up in programmes, procurement and education, where inconsistency can cause friction and confusion.
This is particularly relevant for populations with the least flexibility—children and low‑income families—who depend on institutional food systems more than everyone else.
Ismael Galancho, dietitian (Spain)
Spanish registered dietitian Ismael Galancho, quoted in El Mundo, argues the new pyramid creates a dangerous mismatch between the visual message and the written limits.
Original excerpt: “Hay una cierta incoherencia… si dan protagonismo a la carne roja y los lácteos enteros… Sin embargo, el texto mantiene límites sobre grasas saturadas…”
Translation by foodfacts.org: “There is a certain incoherence… if they give prominence to red meat and whole‑fat dairy… However, the text maintains limits on saturated fats…”
His practical worry is simple: the picture is what most people remember, and the picture suggests red meat and full‑fat dairy are foundational—even if the fine print still caps saturated fat.
Tiffany Bruno, MS, RDN (United States)
Tiffany Bruno (MS, RDN; Switch4Good) focused her feedback on vulnerable populations and food insecurity, warning the inverted pyramid risks nudging low‑income families toward expensive animal foods while pushing affordable staples lower in perceived importance. She points out that beans, legumes and whole grains are often shelf‑stable and cost‑effective ways to meet fibre and micronutrient needs, particularly when fresh produce is hard to access.
Bruno also expects worsening obesity and chronic disease outcomes if the public interprets the pyramid as endorsing animal‑heavy, high‑saturated‑fat eating patterns, arguing it will be “nearly impossible” to stay under saturated fat limits while prioritising animal foods higher in saturated fat—especially concerning for cardiovascular health.
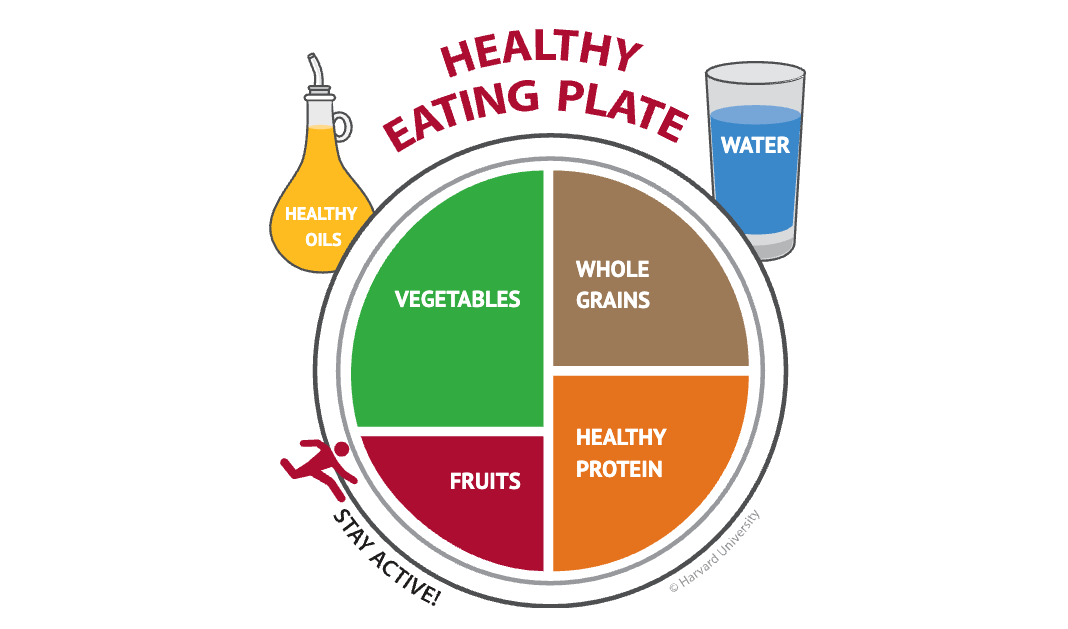
For clients seeking plant‑based patterns for ethical, environmental or religious reasons, she stresses the DGA should not be treated as the “end‑all, be‑all” of nutrition, and recommends looking to other evidence‑based tools such as Harvard’s Healthy Eating Plate.
Where they agree and disagree
Ultra‑processed foods: the biggest area of agreement
Across the reactions, there is broad support for the guidelines’ stronger anti‑ultra‑processed and anti‑sugary‑drink messaging. In this detailed opinion piece, on the recent documentary featuring Joe Wicks, foodfacts.org cofounder Elise Hutchinson makes a similar point: the biggest harms linked with high‑UPF diets tend to come from patterns heavy in sugary drinks, salty snacks, cakes, pastries and processed meats, rather than from every product that falls under a “processing” label.
Harvard’s Healthy Eating Plate also explicitly advises avoiding sugary drinks and prioritising vegetables, whole grains and healthier protein sources, which helps explain why many clinicians use it as a clearer alternative visual.
Protein: “important” isn’t the same as “more”
Dodd’s view reflects a nuance many dietitians recognise: older adults often benefit from higher protein than the RDA, but a blanket 1.2–1.6 g/kg/day message risks being read as “more is always better.” Galancho and Bruno’s concerns add another layer: if people interpret “protein first” as “more red meat,” saturated fat intake can climb quickly, clashing with the guidelines’ own <10% cap.
Looking at things realistically hitting higher protein targets while respecting saturated fat limits tends to push people toward lower‑saturated‑fat proteins, especially legumes and other plant proteins, whether or not the pyramid’s visual communicates that clearly.

Saturated fat: the coherence problem
A repeated criticism is messaging coherence: the document keeps a saturated fat cap while listing butter and tallow as fat options and visually elevating foods often high in saturated fat. That doesn’t automatically make the guidelines “wrong,” but it does increase the chance people will either ignore the cap or assume it no longer matters.
When guidance is designed for mass communication, internal tension is not a small problem, it’s the difference between people following the spirit of the advice and people following the picture.
Equity: what the pyramid means for low‑income families
Bruno’s point is one of the most important: visual guidance can change what families feel they “should” buy, and low‑income households have less room for trial-and-error. If the pyramid nudges families toward expensive animal foods, it can squeeze budgets and reduce purchases of high‑fibre staples (beans, oats, brown rice) that are both cost‑effective and nutritionally valuable.
This is why the translation of guidelines into public programmes matters: the “eat real food” message has very different implications depending on whether someone has time, equipment and access to cook from scratch.
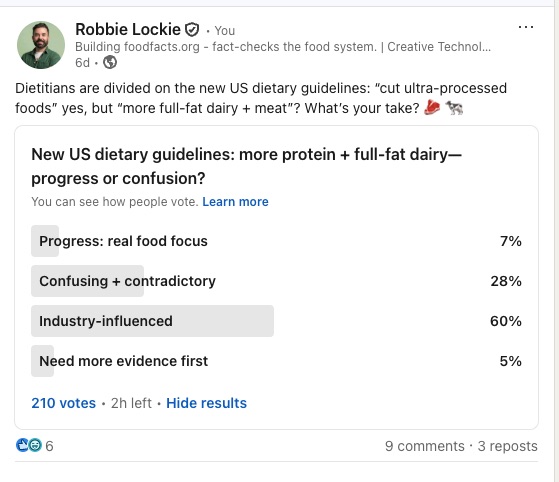
Concerns about industry influence over the new guidelines
The politics of the 2025–2030 Dietary Guidelines have attracted almost as much attention as the nutrition science. Dr Michael Greger, a physician and public health author, captured a widespread suspicion in a single line shared with FoodFacts.org:
“The guidelines were funded by big beef and big butter so no big surprise.”
Formally, the guidelines are funded by US federal agencies, not industry. But recent reporting and conflict‑of‑interest disclosures indicate that experts who helped shape the scientific foundation of the guidelines have extensive ties to meat and dairy interests, raising legitimate questions about how much commercial influence may have coloured a document that strongly elevates protein and full‑fat dairy.
Who sat behind the science?
A STAT (An American science publication) investigation found that several researchers whose work formed the scientific basis for the new guidelines had financial ties to the beef and dairy industries, as well as to major food companies. These ties were disclosed in a scientific report published alongside the guidelines, but critics note that the disclosures were presented as a single combined list for all committee members, rather than person‑by‑person, making it harder for the public to assess how deeply any individual was entangled.
A subsequent Newsweek report reached similar conclusions, noting that multiple authors of the scientific foundation report had received funding or honoraria from organisations including the National Cattlemen’s Beef Association, the National Dairy Council and related trade groups.
From a scientific‑integrity standpoint, industry funding does not automatically invalidate research. But when a guidance document visibly favours the major funders’ product categories—meat and full‑fat dairy—over plant‑based options, it inevitably raises perception and trust issues.
Marion Nestle: “cheerful, muddled… and rife with conflicts”
Nutrition scholar Marion Nestle has devoted a series of essays to what she calls the “MAHA” (Make America Healthy Again) Dietary Guidelines. In her conflicts‑of‑interest post, she writes that it is “startling to observe the industry ties reported by members of this administration’s committee,” especially given the guidelines’ heavy emphasis on eating “protein” (largely understood as meat) at every meal and high‑fat dairy.
After reviewing the disclosures in the scientific foundation report, Nestle points out that:
- Multiple committee members report financial links to meat and dairy trade groups
- These relationships are “surprising in light of the high prioritisation of meat in these guidelines”
- Disclosing conflicts only at the end of the process “isn’t really going to cut it” when the public has no chance to weigh in on panel composition earlier on.

Nestle's broader critique is that the guidelines are “cheerful, but muddled, contradictory, ideological, retro”—cheerful in their “eat real food” rhetoric, but retro and ideological in the way they re‑centre animal‑source foods while sidestepping structural solutions and sustainability.
Formal complaints: “unlawful industry influence”
The Physicians Committee for Responsible Medicine (PCRM), a medical advocacy group that promotes plant‑based diets, has filed a formal petition calling for the guidelines to be rescinded and rewritten, citing what it describes as “unlawful industry influence.”
PCRM argues that:
- Eight of the nine authors of the key scientific report supporting the new guidelines “have received research funding or other remuneration” from beef and dairy industry bodies, including the National Cattlemen’s Beef Association and the National Dairy Council
- This pattern violates the spirit, and potentially the letter, of the Federal Advisory Committee Act, which requires that such advisory processes not be improperly influenced by special interests
Dr Neal Barnard, PCRM’s president, has described the current situation as a “cholesterol cartel” shaping national guidance and called for the guidelines to be rewritten by “impartial authors” who fully centre the latest evidence on plant‑forward patterns, saturated fat and chronic disease.
The US Department of Health and Human Services has defended the process, arguing that experts were chosen through a federal contracting process based on expertise and that all relevant interests were disclosed.
Mixed views from mainstream commentators
Not all observers see the guidelines as entirely captured by industry. A New York Times analysis notes that the guidelines are significantly more critical of the processed food sector than prior versions, with some cardiologists praising the tougher line on ultra‑processed foods and sugary drinks. This has led to a striking juxtaposition:
- Processed-food and sugar‑adjacent industries complain that the guidelines are unfairly harsh on ultra‑processed foods
- Meat and dairy‑critical advocates argue that the same guidelines are too lenient on high‑saturated‑fat animal foods and reflect regulatory capture by those sectors
In other words, criticism is coming from multiple industry directions, not just one.
Why conflicts matter for public trust
From a public‑health perspective, the core concern is not whether every expert with an industry tie is biased, but what these patterns do to public trust:
- When a panel with beef and dairy ties endorses an inverted pyramid that gives pride of place to meat and full‑fat dairy, it becomes harder for the public to believe the guidance is purely evidence‑led
- When plant‑forward patterns—highlighted in the advisory committee’s scientific report and in independent models like Harvard’s Healthy Eating Plate—appear relatively sidelined in the final consumer document, it reinforces perceptions that politics and lobbying have tilted the table
Dr Greger’s comment about “big beef and big butter” further highlights that worry. Even if the formal funding lines run through government, the documented financial enmeshment between panel members and animal‑product industries makes it easier for critics to argue that the guidelines “went in the opposite direction of the science” on plant versus animal protein.
For readers, the takeaway is not to dismiss all guidance out of hand, but to hold two truths at once:
- The new guidelines contain useful, evidence‑aligned elements, especially around reducing ultra‑processed foods, sugary drinks and refined carbohydrates.
- They also emerge from a process where industry influence and conflicts of interest are real and documented, particularly around meat and dairy, and where advisory‑committee science was selectively translated into public‑facing advice.
In that context, using multiple independent reference points—such as Harvard’s Healthy Eating Plate, World Cancer Research Fund recommendations, and high‑quality plant‑based nutrition resources—alongside the DGA can help individuals and institutions triangulate a more robust, less politicised picture of what healthy, sustainable eating looks like.
Practical takeaways (without perfectionism)
- Treat “eat real food” as a direction, not a purity test: build most meals from basics, and be realistic about time and cost.
- If you’re increasing protein, make plant proteins (beans, lentils, tofu, tempeh) your first lever, especially if you want to keep saturated fat under control.
- Don’t let a graphic override the numbers: the saturated fat cap remains <10% of calories even if the pyramid looks butter‑friendly.
- If you’re on a budget, prioritise shelf‑stable staples (oats, beans, lentils, frozen veg) before spending heavily on red meat.
- If you eat plant‑based for ethical or environmental reasons, the new guidelines don't dictate what's healthy for you. Look to resources like Harvard's Healthy Eating Plate instead, they give you a clearer picture of how to build balanced, nutritious meals without animal products.
- Start with high‑impact changes: cutting sugary drinks and ultra‑processed snack patterns often delivers more health benefits than micromanaging small amounts of sugar in otherwise nutritious foods.
- When nutrition content goes viral, slow down and check credentials, incentives and evidence, foodfacts.org’s guide on avoiding online nutrition misinformation is designed for exactly this.

Stand Against Nutrition Misinformation
Misinformation is a growing threat to our health and planet. At foodfacts.org, we're dedicated to exposing the truth behind misleading food narratives. But we can't do it without your support.
Sources + Further Reading
El Mundo (08 January 2026). ¿Qué opinan los nutricionistas de la nueva pirámide nutricional de Trump? El Mundo.
Foodfacts.org (30 October 2024). Avoid false nutrition information online with our practical guide. Foodfacts.org.
Foodfacts.org (31 December 2024). (UPF) Ultra‑processed foods. Foodfacts.org.
Foodfacts.org (18 November 2025). Ultra‑processed foods, plant‑based meat and your health. Foodfacts.org.
Foodfacts.org (15 December 2025). Britain’s junk food trap: how corporate power and ultra‑processed foods shape our diets. Foodfacts.org.
Good Housekeeping (12 January 2026). What dietitians want you to know about the new food guidelines. Good Housekeeping.
Harvard T.H. Chan School of Public Health (Last reviewed January 2023). Healthy Eating Plate. The Nutrition Source.
K‑12 Dive (06 January 2026). New dietary guidelines: More protein, fewer ultra‑processed foods. K‑12 Dive.
Switch4Good (31 October 2025). Tiffany Bruno. Switch4Good.
The Geriatric Dietitian (07 January 2026). The New Food Pyramid and 2025–2030 Dietary Guidelines: What Older Adults Need to Know. The Geriatric Dietitian.
USDA / HHS (January 2026). Dietary Guidelines for Americans, 2025–2030. realfood.gov / Dietary Guidelines for Americans.



Foodfacts.org is an independent non-profit fact-checking platform dedicated to exposing misinformation in the food industry. We provide transparent, science-based insights on nutrition, health, and environmental impacts, empowering consumers to make informed choices for a healthier society and planet.

Was this article helpful?















.svg)
