
Does infant formula cause autism? Why the science says no, and why raw goat’s milk is not a safe alternative





Coral Red: Mostly False
Orange: Misleading
Yellow: Mostly True
Green: True
Learn more about our fact-checking policies
On a recent episode of The Ultimate Human Podcast published on September 23rd, 2025, Gary Brecka discussed a new MAHA report that would soon explore ‘the root causes of autism.’ While the latest U.S.’ government’s announcement focused on acetaminophen (Tylenol), Brecka and guest Barbara O’Neill shifted the conversation toward infant formula and then discussed the suitability of raw goat’s milk for infants who are not breastfed. The podcast team has since clarified to us that given the nature of podcasts, the views expressed in an episode might not necessarily reflect the views of the team or brand itself.
This article checks those claims against the available scientific evidence, and summarises its implications for parents, infants and for public health.
There is no credible evidence of a causal link between infant formula and the development of autism. Autism is a complex condition that is strongly influenced by genetics, with environmental factors playing a secondary role, mainly before birth. For infants who are not breastfed, commercial formulas, whether cow-, soy- or goat-based, are strictly regulated and nutritionally adequate. Raw goat’s milk, however, lacks key nutrients and can transmit dangerous infections, making it unsafe for infants.
Misinformation about infant feeding can have serious consequences. Suggesting that formula is a “driver” of autism risks creating guilt and fear among parents who cannot or choose not to breastfeed. Even more concerning, suggesting raw goat’s milk as a potentially safe substitute could lead to severe nutrient deficiencies and infections in infants. At a time when trust in health guidance is already under pressure, claims like these risk pushing families toward unsafe alternatives.

Be skeptical of messaging that oversimplifies complex conditions or health issues. Credible health advice comes from large-scale research and expert consensus, not anecdotes alone.
What is autism?
Autism or Autism Spectrum Disorder (ASD) is a neurodevelopmental condition, meaning it is related to the way the brain and nervous system grow and develop. Other neurodevelopmental conditions include ADHD and dyslexia.
Autism begins in early childhood and lasts throughout life. It often affects how a person experiences the world, communicates and relates to other people.
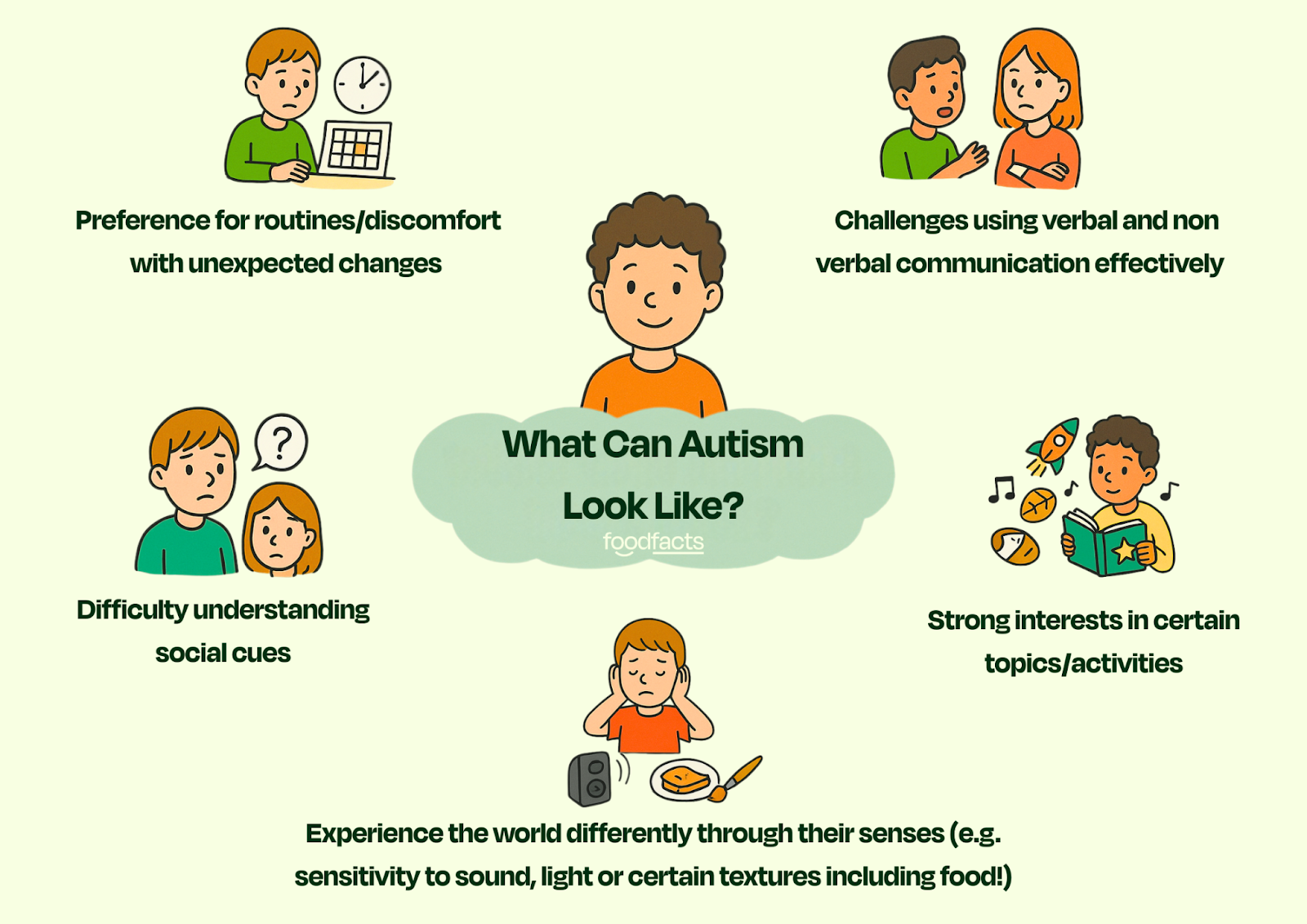
Autism is often referred to as a spectrum as it can vary largely from person to person. Different symptoms, abilities and support needs mean that some autistic people need daily support, while others can live independently.
Despite recent political debates about finding a 'cure', accompanied by negativity in the media, autism is not considered an illness, and is best understood as a difference, according to the National Autistic Society (source). Ongoing research into the causes of autism is not about ‘curing a disease,’ but about better understanding why autism develops, which may help prevent some cases and, just as importantly, improve support for autistic people and their families, especially those for whom autism is profoundly challenging.
What makes it so difficult to establish causation?
There is currently no biological test for autism. Instead it is diagnosed based on observed behaviour.
Autism is complex and highly individualised which makes it difficult to pinpoint a single clear cause. Even in research methods that give us some of the clearest insights, such as twin studies, there are still inconsistent conclusions about the causes of autism (source).
As with many complex conditions where research is still ongoing, a lack of clear answers leaves space for misinformation to spread. Over the years, a wide range of unsupported hypotheses have circulated — from outdated ideas such as “neglectful parenting” (now fully disproven) to more recent claims involving things like acetaminophen, blue light or infant formula.
But what does the evidence actually tell us about the causes of autism? Let's have a further look at the food-related claims and the science behind them.
Claim 1: “I thought the primary driver [of autism] would be vaccination, but it turns out that it's infant formula and blue light coming from screens.”
Fact-check: Although presented as though supported by newer and stronger evidence, this claim is misleading. The phrase 'primary driver' is inaccurate, and there is currently no credible scientific research concluding that infant formula is a cause of autism.
Current evidence shows that genetics play the biggest role in autism. More than 100 genes are already known to increase the likelihood of autism, and many more are expected to be identified in future research (source, source).
The strongest evidence of a genetic component comes from twin studies. These studies compare monozygotic (identical) twins and dizygotic (fraternal or non identical) twins.
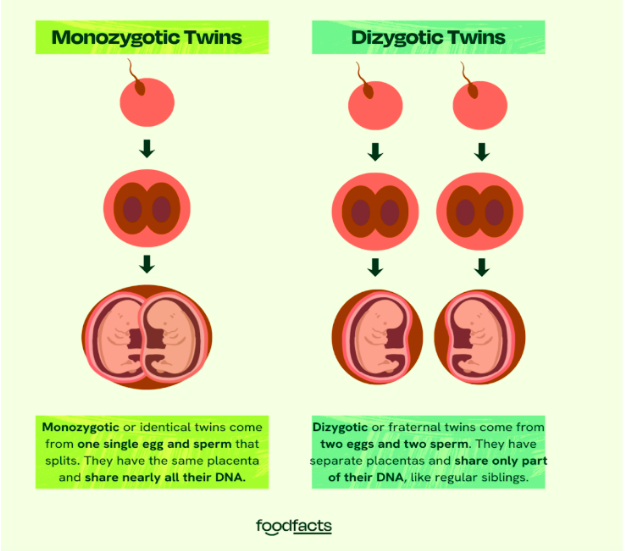
If autism were mostly caused by environmental factors, then we’d expect identical twins and fraternal twins to have roughly the same chance of both being autistic. However, research shows that identical twins are much more likely to both have autism than fraternal twins. This shows there is a strong genetic component.
However, the fact that not all identical twins are both autistic shows that environmental factors also play a role. Most research shows that these environmental factors are mostly prenatal (aka take place before birth) (source). These include things like maternal infection during pregnancy, exposure to certain medications (such as valproic acid), and possibly maternal antibodies. Scientists also study epigenetics (i.e., the way experiences and environments can ‘switch genes on or off’ without changing the DNA itself) as another possible way these early influences might interact with genetics. These influences are less “primary drivers” but rather risk factors that, in combination with genetics, might contribute to autism.
Infant Formula
There is currently no strong scientific evidence that infant formula causes autism. In fact, one large scale study involving over 150,000 children found no significant association between soy-based infant formula and the risk of autism, as well as other neurodevelopmental outcomes such as epilepsy and ADHD (source).
Some studies have reported an association between breastfeeding and lower odds of autism. However, this does not mean that formula feeding causes autism. While associations can be helpful in research, they do not establish causation. This is because there are many confounding factors that can explain those findings. Lifestyle conditions such as socioeconomic status or maternal health may play a role. Reverse causation is another possibility, since early neurodevelopmental differences linked to autism might make breastfeeding more difficult in the first place. Beyond that, breastfeeding and formula feeding differ in ways that go beyond nutrition: breastfeeding involves skin-to-skin contact, hormonal responses, and the natural transfer of bacteria from mother to infant, while formula feeding involves different patterns of interaction. Researchers are exploring whether these differences could influence infant development through epigenetic effects, that is, changes in how genes are switched on or off by early experiences (source). Taken together, these factors mean that one study showing an association does not prove that bottle feeding causes autism.

For example, this study used a large, nationally representative cross-sectional sample (ages 2-5) and found no statistically significant association between breastfeeding and ASD after adjustment for demographic factors. This suggests that any effect, if present, is likely small or confounded by other factors. The authors note that discrepancies between studies may largely be due to differences in how researchers adjusted for confounding variables, and conclude that their findings are consistent with most previous studies having adjusted for confounding factors.
Bottom line
When this limited evidence is considered alongside the strong genetic research on autism, it is clear that infant formula is not a ‘primary driver’ of autism. When a study shows an association between infant feeding practices and the development of autism, more questions need to be asked before definite conclusions can be drawn: how do we know that the use of formula was to blame? What other factors could account for the observed association? These are questions that scientists carefully consider by looking at the overall balance of evidence on a given question before public health guidance might be updated. Misleading claims about ‘primary drivers’ of autism risk not only distorting the science, but also undermining trust in the scientific process itself.
Further consequences of this narrative are guilt among an already very vulnerable group, which could lead parents to turn away from evidence-based care, and to turn to alternatives that aren’t promoted by health professionals or that have been shown to be unsafe. This includes feeding infants raw goat’s milk.
Claim 2: Non-pasteurised, non-homogenised goat’s milk might be offered when breastfeeding isn’t possible.
When asked what advice she would give mothers struggling to breastfeed, Barbara O’Neill starts by suggesting goat’s milk formula. While goat’s milk formula is a regulated and nutritionally adequate option, the discussion implied that raw goat’s milk could also be promoted if it came from a “healthy source” and was prepared with clean utensils.
Fact-check: Following this advice could lead to serious consequences. Infant formulas are carefully regulated to meet babies’ nutritional needs. On the other hand, unmodified goat’s milk is nutritionally inadequate, and raw milk carries serious infection risks (source, source).
Unbalanced nutrient profile
O’Neill claims goat’s milk is ideal for babies because goats are similar in size to human infants. This is misleading. The nutrient composition of milk is shaped by each species’ biology and the growth needs of its young (source), not by how big the animal is.
These differences in needs and milk composition mean that on their own, cow’s milk and goat’s milk aren’t suitable for babies. The protein levels are too high (putting stress on infant kidneys), and they don’t naturally contain the right balance of sugars, vitamins, and minerals that infants need. That’s why formulas made from cow or goat milk are specially processed: they’re diluted and fortified to make them safe and nutritionally complete for babies.
The composition of infant formulas attempts to best mimic that of human milk. For example, while the presence of seed oils in formula is often the target of criticism on social media platforms, and is also the subject of discussion in this podcast, it is important to remember that it is there to provide essential omega-3 and omega-6 fatty acids that are critical for babies’ brain development. For a deeper dive into those issues, check out this related fact-check.
Risk of severe folate deficiency and anemia
Goat’s milk is naturally low in folic acid, and raw/unmodified forms lack essential vitamin fortification (source, source). Case reports show infants fed raw goat’s milk or homemade goat’s milk formula developed macrocytic anemia, a condition where red blood cells are abnormally large but don’t function properly. Other severe complications, including stroke, kidney damage, and life-threatening allergic reactions, have also been reported.

Dangerous infections
The risks associated with the consumption of raw goat’s milk are not merely theoretical: the history of milk-borne disease shows us what can go wrong (source). Raw goat’s milk can carry pathogens such as Q fever (Coxiella burnetii), listeria, toxoplasmosis or brucellosis. These infections are particularly dangerous for infants with immature immune systems. Ironically, while O’Neill and Gary Brecka discuss the importance of gut health and immunity, infections caused by drinking contaminated raw milk could seriously disrupt the gut microbiome and weaken the immune system.
While some studies have observed potential protective effects of raw milk against conditions like respiratory infections, even then the authors stress that such benefits would only be meaningful if the infection risks were eliminated, which is why unprocessed milk continues to be discouraged, particularly in infants.
Bottom line
The scientific literature on reports of complications from infants’ consumption of raw goat’s milk makes it clear that following this advice could have dangerous consequences, and that there remains a lack of awareness regarding the severity of such complications.
O’Neill acknowledged that promoting raw goat’s milk was one of the reasons she was banned from practicing in Australia, following a Health Care Complaints Commission ruling that her advice had the potential to harm vulnerable populations.
Distrust in infant formulas fuelled by such misinformation has also led people to turn to making their own homemade formulas (source), with reports of infants presenting with severe health complications (source).
Beyond the direct dangers of raw milk, these claims reflect a broader narrative that fuels distrust in safe, regulated medical and nutritional practices. When it comes to autism research, oversimplifying the science doesn’t just spread misinformation, it also weakens scientific literacy. Instead of encouraging people to understand how evidence is built and weighed, it stirs up guilt, fear, and confusion. And those emotions can make it harder for parents and the public to trust real science when they need it most.
We have contacted The Ultimate Human Team, who have clarified that the podcast is aimed at encouraging open discussion, and that the suggestions or opinions expressed by guests do not necessarily reflect the brand’s views.
Disclaimer
This fact-check is intended to provide information based on available scientific evidence. It should not be considered as medical advice. For personalised health guidance, consult with a qualified healthcare professional.
Stand Against Nutrition Misinformation
Misinformation is a growing threat to our health and planet. At foodfacts.org, we're dedicated to exposing the truth behind misleading food narratives. But we can't do it without your support.
Sources + Further reading
Sadler, I. (2025). “Can raw milk reduce asthma and allergies in children? A fact-check of recent claims.”
Hutchinson, E. (2025). “Seed oils are in baby formula for a reason. Here’s why it matters.”
National Autistic Society (2025). “Our response to President Trump’s announcement on Tylenol and vaccines.”
Amaral, D.G. (2017). “Examining the Causes of Autism.”
BMJ (2003). “The causes of autism spectrum disorders.”
Ha, E.K. et al. (2021). “Neurodevelopmental Outcomes in Infants Fed with Soy Formula: A Retrospective, National Population-Based Observational Cohort Study.”
Zhan, X-L. et al. (2023). “Infant feeding practices and autism spectrum disorder in US children aged 2–5 years: the national survey of children’s health (NSCH) 2016–2020.”
NHS (2022). “Drinks and cups for babies and young children.”
Basnet, S. et al. (2010). “Fresh goat's milk for infants: myths and realities--a review.”
Borer, K. (2025). “Relevance of Milk Composition to Human Longitudinal Growth from Infancy Through Puberty: Facts and Controversies.”
Baur, L.A. & Allen, J.R. (2005). “Goat milk for infants: yes or no?”
Gosalvez-Tejada, A. et al. (2023). “Multiorgan Failure in a Malnourished Infant: Inappropriate Use of Goat Milk, Dilution, or Both?”
NHS (2023). “Causes - Vitamin B12 or folate deficiency anaemia.”
NHS (2024). “Q Fever”
NHS (2023). “Listeriosis”
NHS (2023). “Toxoplasmosis”
NHS (2023). “Brucellosis”
Gialeli, G. et al. (2023). “Potential Epigenetic Effects of Human Milk on Infants’ Neurodevelopment.”
Currier, R.W. & Widness, J.A. (2018). “A Brief History of Milk Hygiene and Its Impact on Infant Mortality from 1875 to 1925 and Implications for Today: A Review.”
Loss, G. et al. (2015). “Consumption of unprocessed cow's milk protects infants from common respiratory infections.”
Health Care Complaints Commission (2019). “Mrs Barbara O’Neill – Breaches of Code of Conduct – Permanent Prohibition Order.”
Davis, S.A. et al. (2020). “Homemade infant formula recipes may contain harmful ingredients: a quantitative content analysis of blogs.”



foodfacts.org is an independent non-profit fact-checking platform dedicated to exposing misinformation in the food industry. We provide transparent, science-based insights on nutrition, health, and environmental impacts, empowering consumers to make informed choices for a healthier society and planet.

Was this article helpful?
















.svg)
