
Is excess iron a cancer risk? Debunking Dr Eric Berg’s claim with peer-reviewed evidence





Coral Red: Mostly False
Orange: Misleading
Yellow: Mostly True
Green: True
Learn more about our fact-checking policies
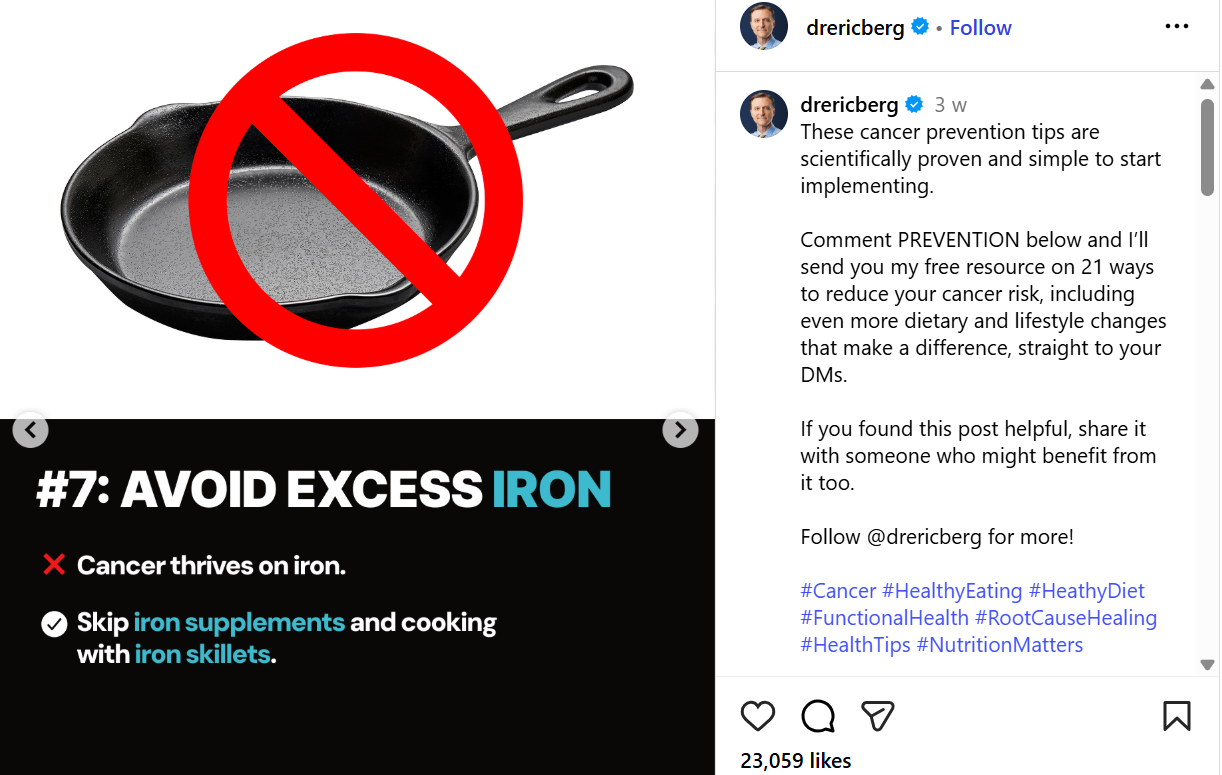
On multiple occasions, most recently on November 11, Eric Berg, D.C., a popular social media health influencer and chiropractor, has repeated claims in widely-shared posts entitled “How to never get cancer.”
Among his “scientifically proven tips,” Eric Berg singles out iron and advises to "avoid excess iron," suggesting that people should skip iron supplements and avoid cooking in iron skillets. Other recommendations include intermittent fasting, following a low-carb diet, and exercising.
This particular tip regarding excess iron appears to have generated significant confusion in the comments, with followers expressing concern as several were prescribed iron for anemia. This fact-check focuses on the implications and scientific evidence behind this particular claim.
Iron metabolism is regulated for most people, and both excess and deficiency may carry risks. There is no evidence linking cast iron to increased cancer risk. The broad advice from this single post is incomplete, and may cause harm if it leads people to skip prescribed treatment.
By using decisive language without context or knowledge of viewers’ health status, social media posts like this risk undermining medical advice and encouraging vulnerable individuals to skip needed treatment through supplementation, potentially worsening health outcomes.

If someone claims something increases cancer risk, check whether they cite credible studies and explain clearly for whom, under what circumstances, and at what dose or exposure this applies. And always be cautious with absolutes like always, never, or the most dangerous; science rarely speaks in extremes.
CLAIM: “Avoid excess iron. Cancer thrives on iron. Skip iron supplements and cooking with iron skillets.”
Fact check: Blanket advice to skip iron supplementation and cookware is not supported by scientific evidence, and omits key context about (1) who is concerned by iron overload, (2) how the body regulates absorption, and (3) the different forms of dietary iron.
Presenting this information without explanation distorts the science and can fuel unnecessary fear. Let’s dig deeper to contextualise those claims.
Where does the claim come from?
The hypothesis that iron can fuel cancer growth dates back to the 1950s, based largely on laboratory models and the fact that iron can act as a pro-oxidant. Excess iron facilitates the production of reactive oxygen species (ROS), which can cause DNA damage, a potential pathway to cancer.
The link between excess iron and cancer is strongest in people with iron overload disorders, such as hereditary hemochromatosis (HH), a genetic condition that causes the body to absorb too much iron. In these individuals, iron accumulates in organs like the liver, where it can drive oxidative stress and DNA damage, significantly increasing the risk of liver cancer (source).

Iron metabolism is tightly regulated
It is important to note that in healthy individuals, iron absorption is tightly controlled. The liver helps control how much iron is in your body by releasing a hormone called hepcidin. When you have enough or too much iron, hepcidin tells your body to stop absorbing more; when you’re low on iron, it allows your body to take in more, keeping your iron levels balanced (source, source). In patients with HH however, hepcidin is inappropriately low or ineffective, leading to uncontrolled iron absorption and iron overload (source).
While excess iron can occur in patients without HH, it is most often due to secondary (acquired) causes such as chronic liver diseases, repeated blood transfusions, or excessive iron supplementation. Indeed this study specifies that iron supplementation “can rarely cause significant iron overload and requires substantial iron intake.”
Experts thus caution against simplified advice found on social media. Nichole Andrews is a registered dietitian with extensive experience working with cancer patients and cancer survivors. She feels that the advice presented in Eric Berg’s post is fear-based, not evidence-based. She further explains:
Research does not support a blanket rule that “iron feeds cancer.” Some cancers alter iron regulation, but this does not mean that removing dietary iron or cookware is protective.
People [who actually need to avoid iron are those] with medically diagnosed iron overload (ex: hemochromatosis) or transfusion-related iron excess. This is rare and always monitored by a clinician. This is not something survivors diagnose themselves from an Instagram post.
Registered Dietitian Aenya Greene concludes: “Dietary iron causing iron overload in healthy people is very rare, because our bodies tightly regulate absorption. Iron overload mainly becomes a concern in conditions like hereditary hemochromatosis, where this regulation is impaired, or when someone takes unnecessary high-dose iron supplements over a long period of time. Your healthcare provider is unlikely to recommend an iron supplement unless blood tests show you genuinely need one. For the majority of people, their diets won’t lead to iron overload. “
Iron and cancer: a nuanced link
Two further crucial aspects are missing from Eric Berg’s post and are essential for interpreting existing research: the types of iron involved, and the potential complications related to iron deficiency, which might warrant supplementation.
Most iron in your body comes from food and exists in two forms: haem iron, found in animal products like meat and fish, is well absorbed; non-haem iron, present in plant foods and supplements, is absorbed less efficiently (source, source).

Some studies have observed modest, positive associations between increased risk of some cancers and higher intakes of haem iron, the type found in red and processed meats (source). It is worth noting that it can be difficult to isolate red meat intake from processed meat intake in studies. While the latter is classified as a Group 1 carcinogen (causes cancer), red meat is classified as Group 2a (probably causes cancer). This article clearly explains what this means and how this translates in terms of risk.
Other studies show that total dietary iron (haem and non-haem), and non-haem iron (from plants, supplements and cookware) are not linked to higher cancer risk and may even be protective (source, source). This means there is no need to avoid haem-rich foods altogether, but rather it is consistent with public health guidelines to limit red and processed meat, eat plenty of plant-based foods, and maintain a balanced diet.
Bottom line
The bottom line here is that if someone broadly recommends avoiding excess iron, without differentiating between the different types of iron, we end up with a distorted picture.
Major cancer prevention bodies, including the World Cancer Research Fund (WCRF) and the American Institute for Cancer Research (AICR), emphasise that overall dietary patterns are what most influence long-term cancer risk. Diets rich in fruits, vegetables, whole grains, and legumes promote iron balance by providing non-haem iron alongside antioxidants and fibre, which help regulate absorption and reduce oxidative stress. This balance helps to keep iron levels within a healthy range.
Indeed the other side of this equation which gets overlooked by the general advice to skip supplementation, is iron deficiency. Low iron levels can lead to anemia, fatigue, and impaired immune function.
Context matters, because when it comes to social media, we don’t know who the readers are. A lot of people who do take iron supplements have been prescribed them by their doctors, following concerns of deficiency. The Global Burden of Disease 2021 analysis estimated that iron deficiency anemia affects over 1.8 billion people globally, making it the most common micronutrient deficiency in the world.
As a result, seeing a post like this one based on incomplete information could easily lead to fear and undermine trust in healthcare professionals, and potentially impact health.
Nichole Andrews calls particular attention to the risks that skipping supplementation could lead to among cancer survivors, calling instead for tailored guidance from professionals:
Iron deficiency is extremely common in cancer survivors. Treatment, blood loss, poor intake, inflammation, and chemotherapy all drive iron deficiency and anemia. Correcting that deficiency improves energy, cognition, strength, and treatment tolerance. Stopping needed iron can worsen fatigue, delay recovery, and reduce quality of life.
Standard oncology guidelines recommend treating iron deficiency, not avoiding iron.
Major cancer groups (ASCO, ESMO, NCCN) emphasize the following:
• Check labs
• Identify true deficiency
• Treat with oral or IV iron when indicated
There is no guideline recommending survivors stop physician-prescribed iron, and no guideline warning against cast iron cookware.
Does cast iron cookware increase cancer risk?
Finally, there is no credible evidence that using cast iron pans or taking appropriately prescribed iron supplements increases cancer risk for the general public. Iron from cookware is poorly absorbed, and in fact cast iron cookware has long been used as a low-cost means to help populations at risk of anemia, particularly in developing countries (source, source).
Final take away
Incomplete advice, such as skipping supplements or everyday cookware, fails to consider who most needs iron (those with anemia, women, pregnant people, cancer survivors) and misrepresents the sources that may increase cancer risk (excess haem iron from red and processed and processed meat). It could also lead to unnecessary fear or even guilt among already vulnerable populations, such as cancer patients and cancer survivors, who are likely to be especially sensitive to messaging framed as proven tips “to never get cancer”.
The big picture: misplaced focus
Overemphasised, decontextualised tips like these can make people anxious, lead to needless dietary restrictions, and obscure what has been shown to reduce cancer risk. Indeed it is important to know that it is a matter of reducing, not eliminating risk.
Ultimately, the most effective route to reducing cancer risk is not micromanaging every micronutrient or following a long list of strict, sometimes unsupported, rules. Rather, it's the same advice consistently championed by experts: eat a balanced diet, rich in varied plant-based foods and moderate in animal products; maintain healthy body weight; engage in regular activity; and avoid tobacco and excess alcohol.
We have contacted Eric Berg and are awaiting a response.
Disclaimer
This fact-check is intended to provide information based on available scientific evidence. It should not be considered as medical advice. For personalised health guidance, consult with a qualified healthcare professional.
Cancer cells use iron. So do your red blood cells, your immune system, your mitochondria, and your recovery pathways.
Avoiding iron without medical indication is harmful for many survivors. Cooking in cast iron is safe.
And no credible evidence supports that dropping iron will “prevent cancer” or “starve cancer.”
The only evidence-based approach:Check your labs. Personalize your plan. Stop letting influencers dictate your medical care.
Stand Against Nutrition Misinformation
Misinformation is a growing threat to our health and planet. At foodfacts.org, we're dedicated to exposing the truth behind misleading food narratives. But we can't do it without your support.
Sources
- Luporsi, E. et al. (2020). “Prevalence of iron deficiency in cancer patients: The French prospective CARENFER study.”
- Richmond, H.G. (1959). “Induction of Sarcoma in the Rat by Iron—Dextran Complex.”
- Fonseca-Nunes, A. et al. (2014). “Iron and Cancer Risk—A Systematic Review and Meta-analysis of the Epidemiological Evidence.”
- Torti, S. V. et al. (2021). “Iron and Cancer.”
- NHS (2020). “Iron”
- BDA. “Iron”
- Waldvogel-Abramowski, S. et al. (2014). “Physiology of Iron Metabolism.”
- Weiss, G. et al. (2021). “Iron metabolism in cancer.”
- Fracanzani, et al. (2001). “Increased cancer risk in a cohort of 230 patients with hereditary hemochromatosis in comparison to matched control patients with non-iron-related chronic liver disease.”
- Gansz, T. & Nemeth, E. (2012). “Hepcidin and iron homeostasis.”
- Bastide, N. et al. (2011). “Heme iron from meat and risk of colorectal cancer: a meta-analysis and a review of the mechanisms involved.”
- Aglago, E. K., et al. (2023). “Dietary intake of total, heme and non-heme iron and the risk of colorectal cancer in a European prospective cohort study.”
- Min, S., et al. (2025). “Iron Consumption and Colorectal Cancer in Korean Adults: A Prospective Cohort Study.”
- NHS (2024). “Iron deficiency anemia.”
- Patrick, K. & Johnson, B. (2024). “Bacon, sandwich ham and salami: How does processed and red meat cause cancer and how much matters?”
- World Cancer Research Fund. “Our cancer prevention recommendations.”
- American Institute for Cancer Research. “AICR's Foods that Fight Cancer™ and Foods to Steer Clear Of, Explained.”
- GBD 2021 Anaemia Collaborators (2023). “Prevalence, years lived with disability, and trends in anaemia burden by severity and cause, 1990-2021: findings from the Global Burden of Disease Study 2021.”
- Sharma, S. et al.(2021). “Effect of cooking food in iron-containing cookware on increase in blood hemoglobin level and iron content of the food: A systematic review.”
- Charles, C.V. et al. (2011). “Iron content of Cambodian foods when prepared in cooking pots containing an iron ingot.”
- Ludwig, H. et al. (2024). “Management of cancer-related anemia.”
- NCCN (2024). “NCCN Guidelines: Cancer- and Chemotherapy-Induced Anemia.”
- Aapro, M. et al. (2022). “Iron supplementation and erythropoiesis-stimulating agents in cancer patients: updated recommendations.”
- ASCO/ASH (2021–2023 revisions). “Clinical Practice Guideline on anemia in cancer.”
- Steinmetz, T. et al. (2022). “IRONOUT: Impact of IV iron in cancer-related anemia.”
- Muñoz, M.; García-Erce, J.A. (2023). “Iron deficiency in oncology.”
- Kowdley, K.V. et al. (2021). “Hemochromatosis and cancer risk.”
- Niederau, C. (2022). “Transfusional iron overload and malignancy.”
- World Health Organization (WHO). (2023). “Iron supplementation and dietary sources.”
- Geerligs, P.P. et al. (2021). “Iron leaching from cookware does not pose a toxicity risk.” International Journal of Food Science & Nutrition.



Foodfacts.org is an independent non-profit fact-checking platform dedicated to exposing misinformation in the food industry. We provide transparent, science-based insights on nutrition, health, and environmental impacts, empowering consumers to make informed choices for a healthier society and planet.

Was this article helpful?

















.svg)
